Menopause marks a significant change in a woman’s life and one of its most common symptoms is fatigue. As we transition through this natural phase, our hormonal balance shifts, often leading to a noticeable increase in tiredness or a feeling of exhaustion that doesn’t seem to improve with rest. It’s not just the end of menstrual cycles that signals menopause; our entire body responds to the decrease in estrogen and progesterone, and these hormonal changes are closely linked to our energy levels.
Understanding the impact of menopause on sleep is crucial because poor sleep quality can exacerbate fatigue. The fluctuating hormone levels can affect sleep patterns, leading to difficulties in falling asleep, staying asleep, or experiencing restorative sleep. Consequently, this disruption in sleep can have a ripple effect, reducing our daytime energy and focus. Addressing menopause-related fatigue involves a multifaceted approach, including lifestyle adjustments and, when necessary, medical interventions. Our overall quality of life can improve significantly by taking steps to manage the fatigue associated with menopause.
Key Takeaways
- Menopause can lead to an increase in fatigue due to hormonal changes.
- Disrupted sleep patterns during menopause contribute to feeling tired.
- Managing fatigue is possible through lifestyle changes and medical support.
Understanding Menopause
In our exploration of menopause, we focus on what it is and the stages it encompasses. Our biological journey is marked by significant hormonal changes that can affect energy levels and overall health.
What Is Menopause?
Menopause marks the end of our reproductive years, signified by the cessation of menstruation for 12 consecutive months. It is a natural biological process, typically occurring in our late 40s to early 50s. The hallmark of menopause is the decline of reproductive hormones, estrogen and progesterone, which can lead to various symptoms and changes in our body. For some of us, menopause may happen prematurely, a condition known as premature menopause, which can occur before the age of 40.
Stages of Menopause
Menopause unfolds in stages, each defined by distinct hormonal transitions:
- Perimenopause: This stage signals the onset, where hormone production from our ovaries begins to fluctuate. Symptoms can include irregular periods and hot flashes. Our fertility diminishes as estrogen levels rise and fall unevenly during this time.
- Menopause: The point when we have not had a menstrual cycle for one year. Our ovaries have significantly reduced hormone production, leading to the cessation of our fertility.
- Postmenopause: After menopause, we enter postmenopause, where symptoms like fatigue may lessen. However, the reduced level of estrogen can have long-term effects on our health, such as decreased bone density.
Understanding the changes in our bodies helps us navigate menopause with confidence.
Symptoms of Menopause
Menopause is a significant stage in a woman’s life marked by the end of menstrual cycles. We see a range of symptoms that vary in severity but are important indicators of this transition.
Common Physical Symptoms
- Hot flashes: A sudden feeling of warmth, usually intense over the face, neck, and chest, leading to sweating and sometimes chills.
- Night sweats: Sweats that happen during sleep can be closely related to hot flashes and often disrupt our sleep patterns.
- Vaginal Dryness: Reduced estrogen levels can result in a decrease in natural lubrication, causing discomfort.
- Irregular Periods: As we approach menopause, the regularity of our menstrual cycle can significantly alter, leading to unpredictable periods.
List of additional common physical symptoms:
- Bloating
- Breast soreness
- Thinning hair
- Frequency of urination
Emotional and Cognitive Symptoms
- Mood Changes: Fluctuations in our hormonal levels can cause variations in our mood, often resulting in quick temperamental shifts.
- Depression and Anxiety: We may experience increased feelings of sadness or episodes of worry that were not characteristic for us before menopause.
- Irritability: A heightened state of frustration or annoyance could become more frequent during this period.
- Brain Fog: Challenges with our concentration and memory, often referred to as “brain fog,” can compromise our usual cognitive functions.
Each of these symptoms may vary in intensity and duration among different individuals, shaping the unique experience of menopause for each of us.
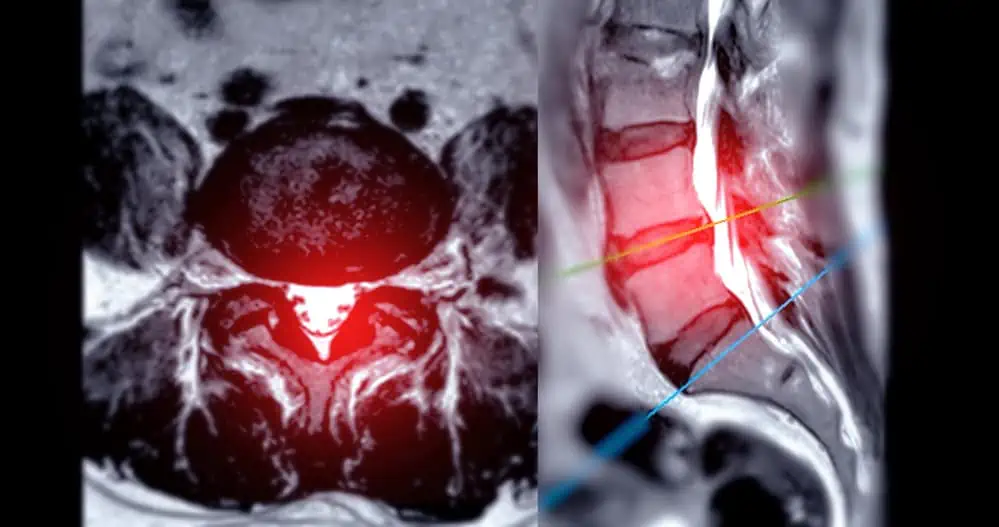
How Menopause Affects Sleep
As we approach menopause, changes in hormone levels significantly affect our sleep patterns, often leading to a decrease in sleep quality and an increase in sleep disorders.
Menopause and Sleep Quality
Menopause can drastically alter our sleep quality. Reduced levels of estrogen and progesterone during menopause can make us more susceptible to experiencing night sweats and hot flashes, which can interrupt our sleep. We often find ourselves waking up throughout the night, which can lead to insomnia or consistent trouble sleeping. To combat these issues, it’s essential to focus on improving sleep hygiene. Here are a few strategies:
- Establish a consistent sleep , aiming to go to bed and wake up at the same time every day.
- Develop a bedtime routine to signal to your body that it’s time to relax and prepare for rest.
Sleep Disorders and Menopause
The prevalence of sleep disorders, such as sleep apnea, also tends to increase as we enter menopause. Symptoms like daytime fatigue are often misattributed to menopause itself, which can lead to these conditions going undiagnosed. A proactive approach, including the potential exploration of cognitive behavioral therapy for insomnia (CBT-I) to address these sleep-related changes, is essential. We should also be aware of the following:
- Increased risk of developing sleep apnea due to hormonal changes.
- Importance of addressing symptoms early with a healthcare provider to get proper treatment and improve sleep quality.
Hormonal Changes and Fatigue
Menopause is a time of significant hormonal changes within our bodies that often lead to increased fatigue. Estrogen, one of the primary hormones affected during this phase, is intricately linked to the regulation of energy levels. Additionally, fluctuations in other hormones like progesterone and cortisol can disrupt sleep patterns and overall well-being, contributing to exhaustion.
Estrogen and Energy Levels
Estrogen plays a vital role in managing our body’s use of energy and the maintenance of stable energy levels. As we approach menopause, our estrogen levels decrease, often resulting in a corresponding drop in available energy. This hormonal change can directly impact our stamina and may cause a feeling of ongoing tiredness.
Other Hormonal Fluctuations
Apart from estrogen, other hormones such as progesterone, cortisol, and melatonin also fluctuate during menopause and affect our energy. Progesterone, which can have a sedative effect, declines alongside estrogen. Cortisol, known as the stress hormone, can interfere with sleep when out of balance, while changing levels of melatonin affect sleep quality. The result of these shifting hormone levels can manifest as persistent fatigue and a decrease in our overall energy reserves.
Addressing Menopause-Related Fatigue
Menopause can significantly impact our energy levels, but with targeted strategies, we can effectively manage fatigue. Addressing this symptom involves both lifestyle modifications and medical interventions tailored to our individual health profiles.
Lifestyle Modifications
We know that incorporating regular exercise into our routine can alleviate some menopause-related fatigue. This might include aerobic activities like walking or swimming, which improve cardiovascular health and can boost energy levels. Strength training is also useful in managing weight gain, which is a common issue during menopause that can contribute to tiredness.
Stress reduction is crucial. Techniques such as meditation and relaxation exercises can help minimize the impact of stress on our energy levels. We should also consider adopting a healthy diet that’s rich in fruits, vegetables, and whole grains to maintain steady energy. Hydration is equally important, so we need to drink plenty of water throughout the day.
Medical Interventions
When lifestyle changes aren’t enough, we may explore medical treatment options. Hormone replacement therapy (HRT) can help stabilize our hormone levels and may alleviate fatigue. However, it’s important to discuss the risks and benefits of HRT with our healthcare provider.
Sometimes, medication such as selective serotonin reuptake inhibitors (SSRIs) might be recommended if our fatigue is linked to mood changes. Supplements like soy lecithin could offer a natural approach, although we should seek professional advice to ensure they’re appropriate for our situation.
For some of us, alternative therapies such as acupuncture have been shown to improve menopause symptoms, including fatigue. While oral contraceptives are usually associated with younger women, they can sometimes be prescribed to manage menopause symptoms due to their hormone-regulating effects.
Making these adjustments can significantly improve our quality of life during menopause. It’s essential to regularly consult with healthcare professionals to find the most effective strategies for managing menopause-related fatigue.
Associated Health Risks
As we navigate through menopause, we’re not just dealing with immediate symptoms—there are also longer-term health risks that may arise. Understanding these can help us take proactive measures to maintain our health.
Long-Term Health Considerations
During and after menopause, we may face an increased risk of several serious health conditions. Notably, our risk for cardiovascular disease goes up significantly. This is partly due to the reduction in estrogen, which is believed to have a protective effect on the heart and blood vessels. High blood pressure is another concern that requires monitoring, as it can lead to heart disease if not managed properly.
Another health risk we must consider is cancer, especially breast cancer, which has been linked with hormonal changes during menopause. Regular screenings and awareness of any family history of cancer are essential for early detection and management.
Diabetes risk also increases during menopause; hence, we should watch our blood sugar levels closely and maintain a healthy diet and exercise regimen to mitigate this risk.
It’s not uncommon for us to experience heightened fatigue during menopause, which, if persistent, can point towards chronic fatigue syndrome or anemia, a condition where we lack enough healthy red blood cells to carry adequate oxygen to our tissues.
We should also be mindful of physical changes like weight gain, which can lead to obesity-related illnesses. A balanced diet and regular exercise can help manage weight.
Lastly, cognitive changes can occur, such as memory lapses or difficulty concentrating. In such cases, approaches like cognitive behavioral therapy can be useful. We’re also susceptible to illness and infections as our immune system may be affected during this time.
By keeping these long-term health considerations in mind, we can seek appropriate preventive care and lifestyle changes to support our well-being during menopause and beyond.
Improving Quality of Life
When addressing menopause-related fatigue, it’s crucial to consider both our emotional and physical health. Implementing strategies to enhance emotional wellbeing and optimizing physical health can significantly improve our overall quality of life during this transition.
Emotional Wellbeing and Support
We know that menopause can be more than a physical journey; it impacts our mental health too. Mood swings and exhaustion can affect our daily lives, which is why emotional support is pivotal. It’s beneficial for us to establish a solid support system, whether that involves talking to friends, joining a support group, or seeking therapy. Managing stress and racing thoughts can also be achieved through mindful practices like meditation or yoga, which help improve our concentration and stabilize our mood.
Optimizing Physical Health
To address physical symptoms like hot flashes and fatigue, we must pay attention to our metabolism and overall health. Keeping our body temperature in check can be as simple as dressing in layers and using a fan. Regular exercise improves our metabolism and can lead to better sleep, while a healthy diet supports hormonal balance. If menopause is disrupting our sleep, we must strive to establish a consistent sleep routine to combat lack of sleep. Additionally, exploring options like hormone replacement therapy, discussed and managed through healthcare providers, has been known to alleviate symptoms like fatigue, headaches, and low libido.
Beyond Menopause
As we move past the menopausal transition, we encounter new health landscapes. The cessation of menstrual periods typically brings a reshaping of our bodily functions, and it’s essential to appreciate the changes and considerations that are particular to this stage.
Postmenopausal Considerations
During postmenopause, our bodies no longer produce the same levels of estrogen. This hormonal change has both immediate and long-term effects on various health aspects, including blood pressure and mental health. The decrease in estrogen can lead to an increase in blood pressure, making it crucial for us to monitor it regularly.
We must also pay close attention to our mental health, as the shift in hormones can influence our mood, possibly contributing to feelings of depression or anxiety. Seeking medical treatment for mental health concerns is as important as addressing physical issues.
Medical treatments and lifestyle adjustments can be necessary even postmenopause to manage symptoms and reduce health risks. Therapies may still include hormone replacement to alleviate symptoms and prevent conditions like osteoporosis.
It’s essential for us to continue regular check-ups in our postmenopausal years to maintain our overall well-being. By doing so, we can address and manage health concerns in a timely manner, ensuring we remain as healthy as possible during our postmenopausal journey.
Factors Affecting The Menopause Transition
As we approach menopause, certain factors significantly impact the transition process. Our diets, nutrition, and substance use all play pivotal roles in how our bodies adjust during this time.
Diet and Nutrition
Our dietary choices directly influence menopause symptoms. Consuming a healthy diet rich in vitamins and minerals helps mitigate some of the discomforts associated with menopause. It is crucial to focus on a balanced intake that includes:
- Fruits and vegetables: Essential for their nutrient content and ability to help balance weight.
- Whole grains: Important for maintaining consistent energy levels.
- Lean proteins: Assist in preserving muscle mass.
Opting for foods that are low in saturated fats and high in fiber can also prevent weight gain, a common challenge during menopause.
Substance Influence
Substances like caffeine and alcohol have noticeable effects on our bodies during menopause. Here’s how they can impact us:
- Caffeine: May exacerbate menopause symptoms like hot flashes and could interfere with sleep, leading to fatigue. It’s advisable to limit caffeine intake to reduce these risks.
- Alcohol: Can trigger hot flashes and contribute to weight gain. It may also affect sleep quality. Moderation is key, and we should be mindful of our alcohol consumption.
In summary, through informed lifestyle adjustments and conscious choices regarding diet and substance use, we can more effectively navigate the journey of menopause.
Conclusion
We understand that menopause is a natural phase in our lives, often accompanied by fatigue which can significantly impact our quality of life. Recognizing menopause fatigue is crucial in managing our daily activities and overall well-being.
- Symptoms: Fatigue during menopause isn’t simply about feeling tired. It’s a profound exhaustion that may not always resolve with rest.
- Management: Adopting a healthy lifestyle, including proper diet and exercise, can reduce the severity of fatigue. Additionally, stress-reduction techniques and ensuring adequate sleep are pivotal.
- Comprehensive Care: Seeking medical advice is important. A healthcare provider might offer hormone therapy or other treatments tailored to our needs, contributing to a better quality of life.
We should embrace this transition with informed choices, supporting each other in seeking care that enhances our lifestyles amidst the changes that come with menopause.
Frequently Asked Questions
In this section, we provide answers to common queries surrounding menopause and its relation to fatigue, offering insights based on factual information.
What are the common symptoms of fatigue related to menopause?
During menopause, fatigue can be experienced as a persistent sense of exhaustion that does not improve with rest. Symptoms may include a lack of energy, reduced motivation, and a decrease in concentration levels. These can be significant enough to interfere with daily activities.
Can menopause contribute to feelings of depression in addition to fatigue?
Yes, menopause can contribute to feelings of depression. Hormonal changes during menopause can affect mood and are often accompanied by sleep disturbances, which can exacerbate fatigue and contribute to depressive symptoms.
What duration is typical for experiencing fatigue during menopause?
The duration of fatigue during menopause varies among women. Some may experience fatigue for a short period, while for others, it might last through the entire menopausal transition, which can extend over several years.
How can diet influence fatigue levels during menopause?
A balanced diet can significantly influence fatigue levels during menopause. Including foods such as soy, which contain phytoestrogens, and maintaining adequate hydration can help manage fatigue.
What treatments are available for managing menopause-related fatigue?
There are various treatments for managing menopause-related fatigue, ranging from lifestyle changes to hormone replacement therapy (HRT). Addressing sleep problems and engaging in regular physical activity are among the initial recommendations.
Is there a link between joint pain and fatigue in menopausal individuals?
Joint pain is another symptom that can accompany menopause and contribute to overall fatigue. Lower estrogen levels are believed to play a role in increased joint pain, which can worsen fatigue in menopausal individuals.