Diagnostic consultations are a fundamental aspect of modern healthcare, forming the cornerstone of patient care. They involve a detailed evaluation where healthcare professionals assess a patient’s symptoms and medical history to determine the underlying causes of health concerns. The success of this process relies heavily on the collaboration between patient and practitioner, and the expert use of diagnostic tools and tests.
In the course of a diagnostic consultation, professionals use their knowledge and experience to navigate through complex symptoms, differentiating between potential health issues to identify a precise diagnosis. This is further supported by cutting-edge technology in medical imaging, laboratory tests, and specialized examination equipment. The process is critical for the effective management of diagnosed conditions and has significant implications for both the prognosis and the treatment options available to the patient.

Key Takeaways
- Accurate diagnostics are key to effective patient care and treatment.
- Health professionals employ a broad range of tools to support diagnoses.
- Ongoing collaboration and training enhance diagnostic processes.
Diagnostic Consultation Overview
In this section, we’ll dissect the intricate practice of diagnostic consultations, emphasizing its imperative for achieving accurate diagnosis.
What Is Diagnostic Consultation?
Diagnostic consultation represents a critical component of clinical practice where we engage with patients to identify their medical condition. The process begins with an initial assessment, often entailing a detailed medical history and physical examination, followed by specific diagnostic tests if necessary. Our objective is to gather comprehensive information that supports an informed diagnosis.
The Importance of Accurate Diagnosis
The quest for an accurate diagnosis is paramount in medicine; it serves as the foundation for effective patient management and treatment strategies. An accurate diagnosis not only guides us in providing proper care but also guards against potential misdiagnoses, which can lead to harmful patient outcomes. In this regard, we rely on a blend of clinical skills, investigative tests, and interdisciplinary consultation to ensure precision in our diagnostic conclusions.
Healthcare Professional’s Role

Our responsibilities in the healthcare system are paramount to delivering accurate and effective diagnostic consultations. We must constantly exercise precise clinical reasoning and maintain a strong partnership with our patients, ensuring their needs and our expert judgment guide our practices.
Clinicians’ Responsibilities
We, as clinicians, bear a critical duty in the medical diagnostic process. Our tasks range from collecting comprehensive patient histories to conducting physical examinations and ordering pertinent diagnostic tests. We must also maintain open communication, providing clear explanations to our patients about their health concerns and the diagnostic steps being taken. It’s imperative that we engage patients and their families throughout this process, as emphasized in a detailed overview of the team-based nature of diagnostics.
Clinical Reasoning and Judgement
When it comes to clinical reasoning, we rely on both analytical and intuitive thought processes. We adopt an evidence-based approach, integrating the latest research and clinical guidelines into our practice. As healthcare professionals, we construct differential diagnoses and synthesize information from various sources, including test results and patient interactions, to arrive at a conclusive diagnosis. A thorough review of clinical reasoning highlights its complexities and importance in ensuring we provide the best possible care. Our ultimate goal is to formulate diagnoses that are timely, accurate, and communicated effectively, leading to optimal patient outcomes.

Patient-Centered Approach
Patient-centered care emphasizes the importance of understanding the patient’s personal experience and fostering clear communication between healthcare providers and patients. We focus on ensuring that caregivers are fully engaged in this process.
Understanding Patient Experience
In a patient-centered approach, we actively seek to comprehend the patient’s experience within the healthcare journey. Patient experience involves their feelings, preferences, and needs as they navigate through the healthcare system. By analyzing the process of inductive foraging, which encourages patients to thoroughly describe their symptoms and concerns, we are better positioned to accurately diagnose and treat our patients.
- We listen intently to the patient’s description of symptoms.
- We consider factors like emotional well-being and life circumstances.
- We aim to understand the full context of the patient’s health.
Communication and Care
Communication and care are the cornerstones of the patient-centered approach, ensuring the delivery of healthcare meets the specific needs of the patient. With a firm foundation in person-centred consultation skills, we ensure that discussions regarding diagnostic and therapeutic options are transparent and collaborative.
- We clarify diagnostic procedures and the rationale behind them.
- We educate patients about their body and health condition.
- We encourage shared decision-making to empower patients.
In our practice, caregivers are equipped with skills to navigate complex conversations, providing patients with all the information necessary to make informed decisions about their diagnosis and treatment. Effective communication leads to better health outcomes and a greater level of trust between us and our patients.
Diagnostic Process
In the diagnostic process, we strive to uncover the underlying cause of a patient’s symptoms through a methodical approach that includes an initial assessment, thorough information gathering, and appropriate diagnostic testing.

Initial Assessment
At the outset, we conduct an initial assessment to understand the primary concerns of the patient. This involves listening to the patient’s description of their symptoms, clarifying their experiences, and noting any relevant factors that could influence their health. We consider this step critical for setting the direction of our diagnostic inquiry.
Information Gathering
Information gathering is the next phase, where we delve into the patient’s medical history, and explore various health-related aspects such as:
- Past medical issues and treatments
- Family health history
- Lifestyle and environmental factors
- Current medications and allergies
This composite of information is crucial for us to form hypotheses about potential diagnoses.
Diagnostic Testing
Finally, we recommend diagnostic testing where necessary to help clarify or confirm our suspicions. Tests may include but are not limited to:
- Blood tests: To assess for infections, organ function, or other metabolic conditions
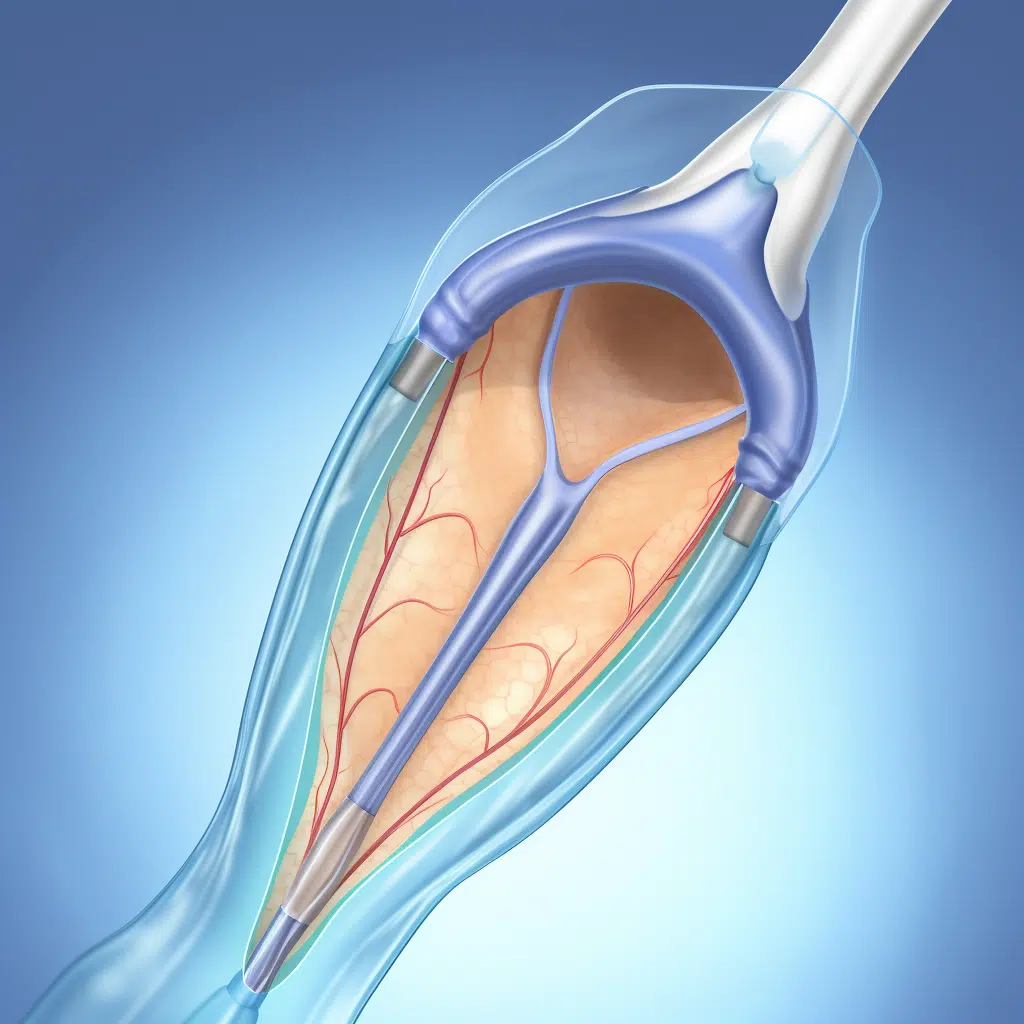
- Imaging studies (e.g., X-rays, MRI): To visualize internal structures and identify any anomalies
- Specialist referrals: For expert evaluations when symptoms are complex or not adequately explained by initial findings
By systematically evaluating the symptoms and data from these steps, we aim to arrive at an accurate diagnosis that will guide effective treatment plans.
Diagnostic Tools and Innovation
In this rapidly evolving field, we see traditional tools being augmented with cutting-edge technologies, including artificial intelligence, to enhance diagnostic accuracy and patient outcomes.

Traditional and Advanced Diagnostics
The spectrum of diagnostic tools has broadened significantly from the staples of X-rays and lab tests to include MRIs and CT scans, offering a more detailed view of the human body’s internal structures. The advancement in diagnostics has not only improved the resolution of these images but has also resulted in innovations like portable devices, facilitating diagnoses in a variety of settings outside traditional clinics.
- X-rays: Still widely used for their speed and cost-effectiveness.
- MRIs: Offer greater detail for soft tissue evaluation.
- CT Scans: Provide cross-sectional views and are vital for diagnosing complex conditions.
The Role of Artificial Intelligence
Artificial intelligence is revolutionizing how we approach diagnostics. AI algorithms can analyze medical imaging with a high degree of precision, often identifying subtleties that may be overlooked. For instance, in radiology, AI-enhanced tools assist in interpreting CT scans and MRIs, reducing the time to diagnosis and helping to prioritize critical cases.
- Precision: AI algorithms provide meticulous analysis, capturing details human eyes might miss.
- Speed: AI significantly cuts down the time required for reviewing and interpreting medical images.
By integrating AI into diagnostic practices, we are not just innovating; we are redefining the standards of care and opening up new possibilities for early and accurate diagnosis.
Common Challenges in Diagnostics

When exploring the intricacies of diagnostic consultations, we encounter a range of challenges. These challenges can impact patient safety, raise ethical questions, and require strict adherence to regulatory standards. Our deep understanding facilitates a clearer view of these issues.
Diagnostic Errors and Uncertainty
Diagnostic errors and uncertainty represent a significant challenge in clinical practice. Patient safety is at risk when a diagnosis is incorrect or delayed. Notably, we must recognize the complexity of symptoms that often masquerade as common ailments, potentially leading to misdiagnosis. For instance, a patient presenting symptoms of a urine infection could, in reality, have pneumonia, which if not diagnosed correctly, can lead to severe patient safety concerns.
- Prevalence: Studies indicate that diagnostic errors occur in a notable percentage of primary care consultations.
- Resolution: Discussion of diagnostic uncertainty early in the clinical visit may lead to resolution by its end.
Ethical Considerations
In our pursuit of diagnostic accuracy, ethical considerations play a central role. We must navigate patient confidentiality and the moral obligations involved in the disclosure of diagnostic uncertainties. This affects how we communicate with patients, requiring a balance between honesty and maintaining hope.
- Communication: Limited communication of diagnostic uncertainty can impact trust and decision-making.
- Decision-making: Ethical challenges arise when we respect patient autonomy while ensuring informed decisions.
Regulatory Compliance
Adherence to regulatory compliance, including data protection laws, is a stringent requirement for us. Regulations mandate the safeguarding of patient information and upholding quality standards in diagnostic processes.
- Data Protection: We must ensure patient information confidentiality and security.
- Standards: Our adherence to clinical standards is critical for accurate and safe diagnosis.
We continuously strive to improve diagnostic consultations, acknowledging these challenges and responding with strategies designed to promote positive patient outcomes.

Clinical Education and Training
In our pursuit of excellence in healthcare, we recognize the central role that systematic and evidence-based education and training play in shaping the competencies of medical professionals, from medical students to experienced practitioners. These efforts are directly linked to improving clinical outcomes.
Medical Students and Novice Clinicians
For medical students and novice clinicians, the foundation of diagnostic skill starts with a rigorous curriculum. We integrate key competencies into our educational programs that encompass not just individual knowledge and skillsets, but also teamwork and systems-based practice. These competencies include clinical reasoning, patient communication, and an understanding of diagnostic workflows. We align our strategies with best practices, as highlighted in the discussion on educational outcomes of a national consensus project.
Ensuring that our novice clinicians perform effectively in the diagnostic process calls for a curriculum that balances theory with practical exposure. The transition from understanding disease processes to applying that knowledge in clinical settings represents a critical leap. Our education methods, therefore, include case-based learning, simulations, and supervised clinical rotations. These methods help bridge the gap between academic understanding and real-world diagnostic acumen.
Continuing Professional Development
Continuing professional development (CPD) is imperative for maintaining competency and improving diagnostic practices among healthcare professionals. Our CPD programs are designed to address areas like clinical reasoning and diagnostic teamwork. By introducing current, evidence-based information, we promote lifelong learning and continuous improvement.
Our CPD initiatives focus on enhancing the diagnostic process by offering courses that update practitioners on the latest diagnostic methods and technologies. Through these programs, we aim to fortify the link between ongoing education and tangible improvements in clinical practice. Collaboration and communication within the clinical team are encouraged, recognizing their essential roles in strengthening diagnostic accuracy, as described in a policy brief on education and improving diagnosis.
Through these structured educational endeavors, we maintain our commitment to improve the care our patients receive by continually equipping our professionals with the knowledge and skills necessary to achieve accurate diagnoses.
Interdisciplinary Collaboration

In the arena of diagnostic healthcare, we understand that the most effective patient outcomes are often achieved through interdisciplinary collaboration. This approach leverages diverse expertise to develop a comprehensive diagnosis and an integrated care plan.
Multidisciplinary Approach to Diagnosis
In the realm of diagnosis, the value of a multidisciplinary approach is undeniable. We gather experts from various disciplines to collectively analyze a patient’s case, leading to more accurate and holistic assessments. In this process, individuals such as radiologists, pathologists, and specialists in relevant fields come together to discuss, debate, and decide on the diagnostic conclusions.
- Radiologists provide crucial imaging insights.
- Pathologists confirm disease presence and stage.
- Specialists contribute nuanced understanding of complex conditions.
This cross-pollination of knowledge ensures that we don’t miss subtleties that might elude a single-discipline perspective.
Referral Systems in Primary Care
When we consider the referral systems in primary care, our goal is clear: streamline the transition from initial consultation to specialized assessment. The referral pathway starts with primary care physicians who are often the first point of contact for patients.
- Identify Need: We assess symptoms that require specialist input.
- Choose Specialist: Referrals are based on the patient’s specific conditions.
- Coordinate Care: We maintain constant communication to ensure continuity of care.
Through this structure, patients are directed to the most appropriate specialists, guaranteeing that every condition is addressed with the right expertise.
Quality and Outcome Measurement
When we discuss the quality and outcome measurement in diagnostic consultations, we focus on the accuracy of diagnoses and the consequent effects on patient health and quality of life.
Evaluating Diagnostic Quality
We recognize that diagnostic quality is pivotal as it forms the foundation for effective treatment plans. It is critical to assess the diagnostic accuracy which can be achieved by implementing standardized quality indicators that gauge the precision of the diagnostic process. For instance, we may review the correlation between proposed diagnoses and the eventual confirmed conditions. Likewise, implementing peer reviews and case audit systems ensures continuous improvement in diagnostic practices.
- Peer Review: Involves the assessment of diagnostic methods and decisions by fellow clinicians.
- Case Audits: Entail a systematic review of patient cases to identify trends and deviations in diagnostic accuracy.
Patient Outcomes and Life Quality
Patient outcomes directly reflect the impact of clinical interventions on their health status. We observe the clinical outcomes to determine the effectiveness of our diagnostic proficiency. Quality of life, another important marker, hinges not only on health improvements but also on the patient’s capacity to engage in day-to-day activities post consultation.
- Clinical Outcomes: Measured by tracking recovery rates, morbidity, and mortality statistics.
- Quality of Life: Assessed using patient surveys that examine the physical, emotional, and social aspects of a patient’s well-being post-diagnosis.
By adhering to these measurement parameters, we uphold our commitment to providing high-quality diagnostic consultations that aim to elevate patient health outcomes and life quality.
Specialized Areas of Diagnosis
In modern healthcare, we recognize the importance of specialized areas of diagnosis to cater to the varying complexities of diseases. Each specialty demands a comprehensive understanding and precise diagnostic processes to ensure effective patient care.
Neurology
Neurology is crucial for diagnosing and managing conditions related to the nervous system, which includes the brain, spinal cord, and nerves. For example, in cases of chronic pain or back pain, it is essential to determine whether the cause is neurological. Detailed neurological examinations and imaging techniques are utilized to pinpoint disorders such as multiple sclerosis or Parkinson’s disease.
Cardiology
The field of Cardiology is dedicated to diagnosing heart and blood vessel disorders. Diagnostics in cardiology often involve echocardiograms, electrocardiograms (EKGs), and stress tests to detect heart abnormalities. We are committed to advancing our understanding and technology to tackle cardiac diseases effectively.
Pediatrics
Pediatrics focuses on the diagnosis and treatment of medical conditions affecting infants, children, and adolescents. This field requires special consideration of developmental stages and how diseases manifest differently in children compared to adults. We employ a range of diagnostic tools from simple physical assessments to advanced imaging, depending on the child’s symptoms and needs.
Management of Diagnosed Conditions
After a diagnosis is confirmed, we focus on the effective management of the condition. This includes formulating a treatment plan tailored to each individual’s needs, and regularly monitoring and reassessing their progress to ensure optimal care.
Treatment Planning and Management
We craft a treatment plan that serves as a blueprint for managing diagnosed conditions. Our treatment plan specifies the types of medications, therapies, and lifestyle adjustments necessary for managing symptoms, including pain management strategies for those dealing with chronic pain. We prioritize treatments aimed at providing relief and improving quality of life, while being cautious to avoid unnecessary interventions that might lead to complications.
- Medications: Prescribe appropriate pharmaceuticals for symptom relief and disease management.
- Therapies: Identify suitable physical or cognitive therapies for comprehensive care.
- Lifestyle Changes: Advise on diet, exercise, and other modifications to support treatment.
Monitoring and Reassessment
Continuous monitoring is crucial for us to evaluate the effectiveness of the treatment plan. We conduct regular reassessments to ensure the management strategy remains aligned with the patient’s evolving health status.
- Clinical Assessments: Schedule periodic reviews to observe symptom progression or improvement.
- Feedback Loop: Encourage patient feedback to understand their experience with current management strategies.
- Adjustments: Make necessary adjustments to treatment plans based on ongoing evaluations and patient response.
Future Perspectives
In this section, we’ll explore the transformative shifts and the pivotal role that diagnostic technologies will play in shaping the future of healthcare.
Emerging Trends in Diagnostics
Recent systematic reviews and studies signal a paradigm shift in diagnostic solutions. We are witnessing a surge in innovation that is making diagnostics more rapid, accurate, and accessible. Point-of-care testing and wearable diagnostic devices are becoming more prevalent, promising real-time health monitoring and immediate results. Advances in molecular diagnostics are also enabling more personalized approaches to treatment, moving us closer to the goal of precision medicine.
The Future Role of Diagnostics in Healthcare
As we look toward the future, our vision is informed by current ventures and support from entities like the National Institutes of Health. The integration of diagnostic technology with telemedicine will likely redefine the convenience and efficiency of healthcare services. We anticipate that diagnostic platforms will evolve to not only detect diseases but also to predict and prevent them, pivoting the healthcare system from reactive treatments to preventive health management. This future of diagnostics, driven by continuous innovation and patient-centered approaches, will enrich our ability to make informed decisions and manage health outcomes effectively.
Frequently Asked Questions
In this section, we address some of the most pertinent questions related to the diagnostic process and consultation in healthcare.
What are the essential steps involved in the diagnostic process?
The diagnostic process often starts with taking the patient’s history, followed by a physical examination. Diagnostic testing may ensue based on initial findings to confirm a diagnosis.
What constitutes a comprehensive medical consultation?
A thorough medical consultation includes discussing patient history, understanding current symptoms, analyzing previous medical records, and formulating a plan for diagnostic procedures as necessary.
How do diagnosis and consultation differ in a clinical setting?
Diagnosis is the process of identifying a disease or condition, while consultation is broader, involving patient interaction, examination, and discussion of treatment options post-diagnosis.
What are the primary types of diagnostic testing used in healthcare?
Common diagnostic tests include imaging studies like MRI or CT scans, blood tests, biopsies, and specialized tests such as genetic testing depending on the suspected condition.
Why are diagnostic services critical for effective patient care?
Diagnostic services are crucial because they provide the necessary information to determine the appropriate treatment plan, facilitating timely and targeted medical interventions.
What guidelines should be followed during a medical consultation for accurate diagnosis?
To ensure accuracy, guidelines include adequate patient preparation, clear communication, and comprehensive examination. This may involve educating patients on what to expect and how to prepare for their consultation.